Walter is a 57 year old man who presents with a left neck mass. He first noticed it about 2 months ago, and it has slowly gotten bigger since then. It is hard “like a rock” but is not painful. On further questioning, he says that he has also been having left ear pain for the past few months. He denies any change in voice, difficulty swallowing, difficulty breathing, or coughing up blood. He has lost 15 pounds in the past several months without actively dieting- he just has less appetite.
His past medical history is notable for high blood pressure. He had surgery over 20 years ago after breaking his leg in a car accident. He currently takes a blood pressure medication and over the counter allergy medications as needed. He has smoked 1.5 packs of cigarettes daily for the past 40 years. He drinks less than 5 beers per week but was “a big drinker” when he was younger.
His head and neck exam is notable for an irregular, ulcerated mass in his left tonsil.
Additionally, he has a firm approximately 3 cm left upper neck mass with no other palpable masses in the neck on either side. Fiberoptic endoscopy shows that the left tonsillar mass also involves the left base of tongue. The remainder of the pharynx and larynx appear normal and both vocal cords move normally.
Walter had a biopsy taken from the left tonsil mass in the office which confirmed the diagnosis of squamous cell carcinoma. While waiting for the biopsy results, he had radiographic imaging done: a CT scan of his neck and of his chest. The neck scan showed a 3.5 cm mass based in the left oropharynx (tonsil and base of tongue) as well as a 4.5 cm left neck lymph node which appeared to be infiltrated with cancer. The chest CT scan showed no sign of cancer spread into the chest.
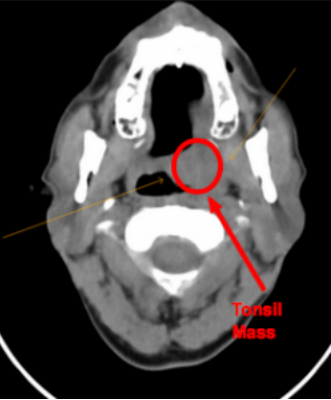
CT showing the left tonsil mass
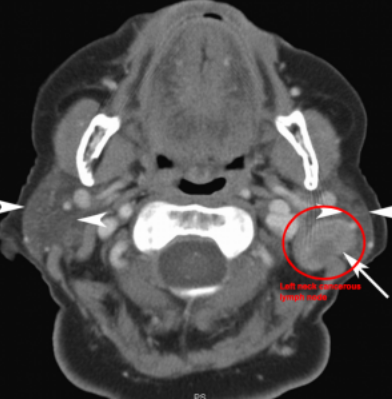
CT showing the cancerous left neck lymph node
A staging endoscopy of the mouth, throat, and esophagus was performed under anesthesia. The goal of this procedure was to get a better idea of the limits of the left tonsil mass and to closely examine the throat and esophagus for any additional tumors.
At this point, Walter was staged as a T2 N2A M0 squamous cell carcinoma of the left oropharynx. He was seen by a radiation oncologist and medical oncologist for evaluation and then these specialists and the ENT surgeon discussed the patient and offered recommendation for treatment. It was recommended that Walter undergo combined chemotherapy and radiation treatments. Although surgery was also an option, this would require an extensive resection and reconstruction with significant risk of permanent swallowing problems after surgery.
Walter elected to proceed with chemoradiation. Prior to starting treatment, a gastric feeding tube was placed. This is a rubber tube that goes straight through the skin of the belly into the stomach. It is very common that patients undergoing radiation treatment to the throat are unable to swallow temporarily during the treatment. For this reason, it is recommended that they have a feeding tube placed so they can continue to get adequate nutrition. In addition, Walter had very poor teeth, with multiple missing teeth already. He was seen by a dentist and had his remaining teeth pulled prior to radiation treatment.
For his treatment, Walter had radiation given daily Monday through Friday for about 6 weeks. He also had weekly doses of chemotherapy. Although the treatment caused only mild side effects the first week or two, by the last weeks of the treatment, he was having significant pain, irritation of the lining of his mouth and throat, and skin redness with areas of breakdown.
After completing the treatments, significant shrinkage of the tumors in the throat and neck were noted. On his post-treatment CT/PET scans 3 months after completing treatment, there was no sign of surviving cancer in either the throat or neck.
Walter gradually regained his ability to swallow and the feeding tube was removed. He continued to have dry mouth, mild difficulty swallowing, and a scarred “woody” appearance of his neck skin (these are all typical side effects of radiation).
He was seen monthly the first year after treatment, then every other month the next year, and every third month the third year. He is now over 3 years out from his treatment and is cancer free. He quit smoking at the time of his diagnosis. He will continue to be monitored on a regular basis (will get less and less frequent as time goes on without any cancer recurrence).
In conclusion, Walter’s story is a pretty typical “success story” for someone with head and neck cancer. Even with the success stories, the treatment for these cancers is difficult and carries substantial side effects. The best treatment for head and neck cancer is prevention- quitting smoking (or never starting!) and avoiding excessive alcohol drinking. Recently, HPV-associated throat cancers have been increasing, so people may want to consider getting vaccinated against HPV to lower their risk of oropharyngeal cancer.



