The American Migraine Association estimates 36 million people in the United States suffer from migraines, and many more have not been diagnosed. These debilitating headaches are triggered by a wide range of causes, and some doctors think they may be connected to sleep disorders.
Migraines
A headache that keeps a person from his daily activities, is accompanied by sensitivity to sound or light, and lasts from 4 to 72 hours, falls into this category after the fifth episode. Although other symptoms, such as pulsated throbbing, nausea and auras are often associated with the pain, they are not part of the diagnostic criteria. Some may, in fact, be more like tension headaches.
Most researchers now think the cause is genetic one that results from hypersensitive brain cells in the nervous system. Triggers include sudden changes in hormone levels, certain foods or additives, stress, medication and environmental factors. Females and people with family history are more likely to develop this kind of headache, and they often start during adolescence. A person who has symptoms 15 or more days a month for three months has a chronic condition.
Sleep Apnea
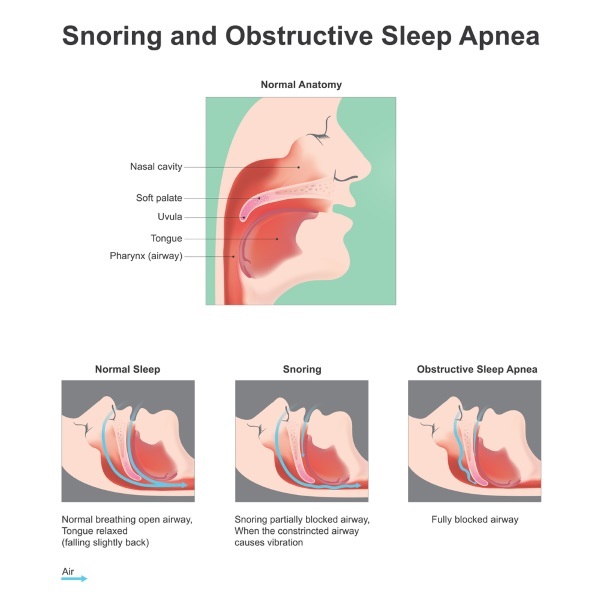
Sleep apnea is a sleep disorder that causes a person to repeatedly stop breathing for short amounts of time during sleep. Signs include loud snoring and feeling tired after getting a full night of sleep. People with sleep apnea may also gasp for air, have insomnia, or have trouble paying attention during the day. Apnea can cause daytime accidents, complicate illnesses like heart trouble and diabetes, and interfere with medications. It may also lead to sleep apnea headaches.
There are three kinds of sleep apnea. Obstructive sleep apnea takes place when the throat muscles relax during sleep and obstruct the airways. Central sleep apnea occurs when the brain signals to the muscles don’t work properly. The third kind is a combination of obstructive and central apnea.
Sleep Apnea Headache vs Migraines
People who have sleep apnea often have morning headaches, but the connection works both ways. People with other types of headaches may also be at risk for sleep apnea. In a 2017 survey, 37 percent of the participants with headaches were also at high risk for sleep apnea, a rate not seen in the general population. Other studies show that around 50 percent of the people with morning headaches probably also have sleep apnea.
Migraines often have the following characteristics:
- Accompanied by sensitivity to light and sound
- Cause nausea and vomiting
- Usually occurs on one side of the head
- Are accompanied by visual problems
- Last from hours or days
Sleep apnea headaches usually cause these symptoms:
- Go away when normal breathing returns
- Occur on both sides of the head
- Reoccur on a regular basis
Three kinds of headaches are associated with sleep apnea: cluster, hypnic and obstructive sleep apnea (OSA). Cluster headaches come in patterns over a period of days or weeks. Hypnic headaches involve intense throbbing that interrupts sleep. OSA headaches occur when blood vessels widen and oxygen levels drop.
Anyone who has frequent headaches should see a medical professional for diagnosis and treatment. It takes a trained eye to distinguish between sleep apnea headache vs migraines.